What’s in it for me?
Children and Coronavirus Infection: What’s so different about this cohort?
Dr. Nabeel Akram
A 5-year old boy, Jian, visited his grandparents in Hubei province China in January earlier this year. On the second day after their arrival, Jian, his 10-year-old sister Mei, and their parents went to the shopping mall, watched a movie at a theater and then came back home for dinner together with the rest of his family. Jian’s grandparents, in their 70s, did not go with them. Jian’s grandfather also had hypertension and diabetes for the last 12 years and he has been on medication since then. After 3 days, Jian’s grandparents and parents gradually showed signs of flu with persistent dry cough, fever and body aches. After testing it was confirmed that the family got infected with novel coronavirus including Jian and Mei. However, Jian did not show any symptoms while Mei only had a mild cough that subsided in a couple of days. While Jian’s parents also showed improvement in 5-7 days with the use of over the counter anti-analgesics and antipyretics, the grandparents’ health deteriorated over time and needed hospitalization. They were quarantined and later on diagnosed and treated for pneumonia. While Jian’s grandmother was still in a critical condition with pneumonia, his grandfather eventually died since he developed pulmonary complications along with complexities with his co comorbidities; his lungs got weaker and weaker and eventually, he could not survive despite being on the ventilator support. The family was separated to prevent the spread of infection and the grandfather could not see his children or grandchildren since a few days before he died. After 15 days from the onset of the first symptoms in Jian’s parents and grandparents, Jian still did not show any symptoms of flu, even when he was tested positive for coronavirus along with the rest of his family.
This is one of the hypothetical scenarios constructed based on some of the case series reported so far in the scientific journals such as The Lancet, New England Journal of Medicine (NEJM) and Journal of American Medical Association (JAMA) from several hospitals in China and particularly from Wuhan, China and Lombardy area in Italy. The transmission of infection in family clusters has been one of the most commonly reported modes of spread. Researchers, physicians and medical staff in China, Italy and other early-affected countries have been doing a great service in publishing case studies that is helping other countries to prepare and find solutions for the outbreak. As more and more data is reported every day, the leading scientific journals are publishing data at an increasing pace now and making coverage of coronavirus research articles available to a wider audience through their free online access.
Why Jian did not present with any symptoms when he had more or less similar exposure to the virus and was infected with it like the rest of his family? Why did different family members in different age groups give a different presentation of symptoms? As much as these questions are perplexing and puzzling for the scientific community, the answers to these questions could provide invaluable clues for the development of the solutions for this serious and unprecedented outbreak of what is commonly known as coronavirus.
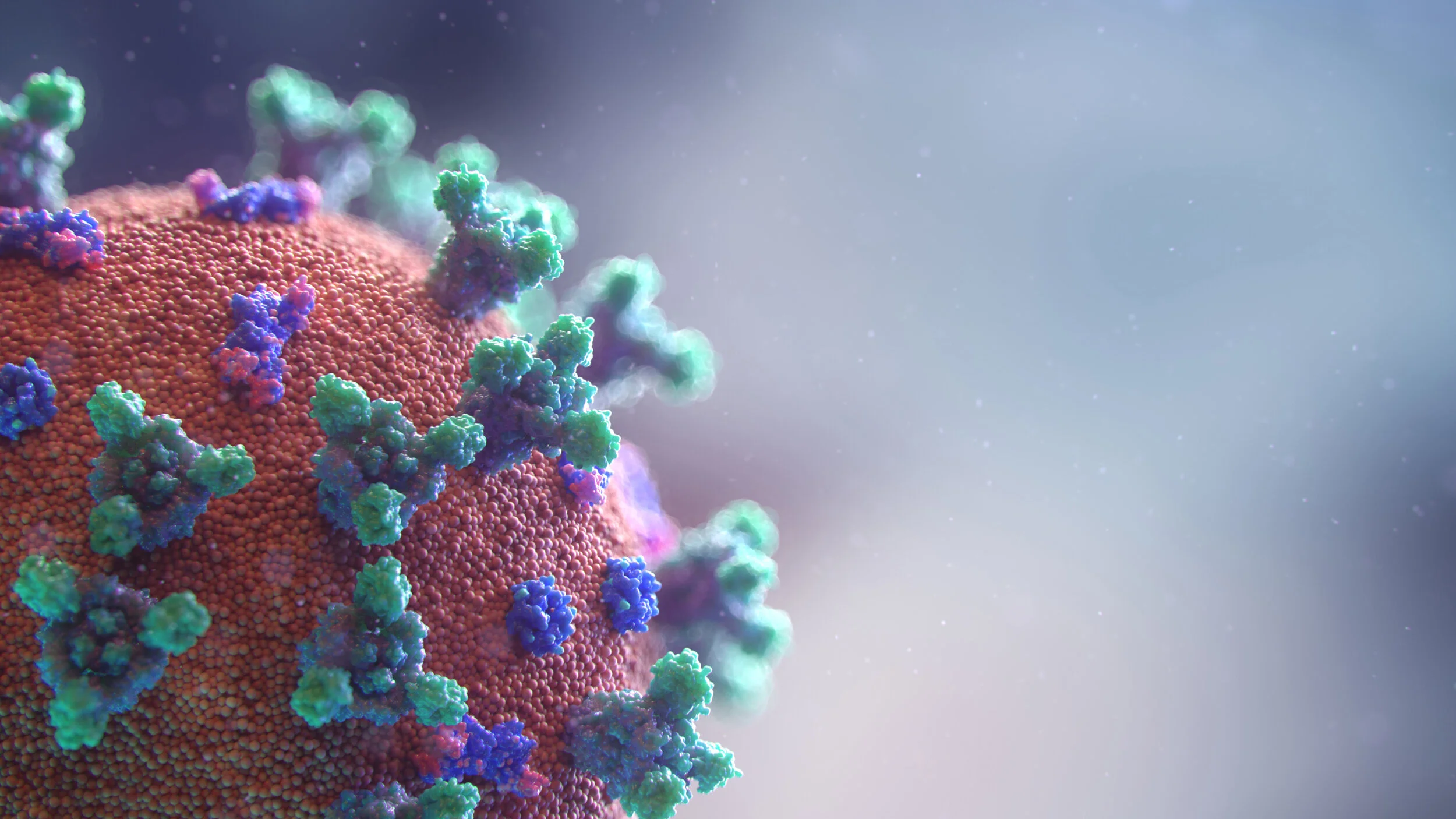
For the purpose of clarity, the virus causing this havoc globally is SARS CoV-2 (Severe Acute Respiratory Syndrome Corona Virus 2) and the disease manifested as a result of its infection is called COVID-19 (Corona Virus Infectious Disease 2019).
“As much as these questions are perplexing and puzzling for the scientific community, the answers to these questions could provide invaluable clues for the development of the solutions for this serious and unprecedented outbreak of what is commonly known as coronavirus.”
If we look back and analyze the data of previous viral outbreaks such as SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome) – the pattern is more or less the same and the children critically affected by these outbreaks are also handful as compared to the adults, especially if compared to the elderly with other morbidities.
According to WHO, in the current outbreak so far, China has reported 2.4% cases and of these only 0.2% children under 10 were critically ill. Only recently, there is one reported case of an infant dying of the coronavirus as compared to 21.8% fatality rate for cases 80 years and over. The same indicator for adults between the ages of 10-39 years is only 0.2%. Similarly, in SARS of 2002, there were 774 fatalities and none of them was a child, while in MER since 2012, there are 858 deaths attributed to the disease with very few children with disease symptoms.
The typical symptoms of COVID-19 can appear 2-14 days after exposure to the virus and consist of fever, dry cough, and dyspnea or shortness of breath. A severe illness leads to pulmonary complications with inflammation of lungs due to infection (pneumonia) resulting in weakness of lungs requiring a ventilator or other pulmonary support. Failure to restore lung functions can eventually lead to death.
We know from previous studies that the incidence of lower respiratory tract infections plotted on a chart by age groups shows a U-shaped pattern. There are more respiratory infections resulting in pneumonia or weakness of lungs in either infants or children and then we see the number rising again as the cases are older and in 60 plus age range. In COVID-19, however, we see more of a J-pattern than a U-shape. The upper left arm of U is not there in the case of coronavirus infection when it comes to COVID-19. That is perplexing for scientists.
There is no definite answer to this question yet but there are some hypotheses presented by various scientists that need further investigation. These hypotheses are either related to the immune response of individuals at different ages or related to host factors.
Cytokines are proteins in the human body that are produced by cells and they behave like the messengers between these cells. These cytokines play an important role in a response to any inflammatory episode. One of the common complications of COVID-19 is acute respiratory distress syndrome or ARDS affecting the lungs, causing pneumonia and creating an inflammatory episode. In adults, there is an aggressive immune response to this inflammation and the cytokines are released in large numbers, causing what is commonly known as a Cytokines Storm. Think of a situation in which an army is called in for a neighborhood bicycle theft. This sudden surge in cytokines could be damaging to the lungs. The response is even more pronounced if the patient has comorbidities such as respiratory or cardiovascular disease. In older patients, such a Cytokines Storm can cause enough damage to the lungs to make them much weaker and susceptible to more severe lung conditions such as pneumonia and eventually the patient has to be put on pulmonary support like ventilators. Scientists believe that in children such a response to infection or inflammation is not as developed and Cytokine Storm is not as pronounced. The infection from coronavirus ends up being not as severe in young, as in adults, and thus preventing their lungs from being damaged.
“Think of a situation in which an army is called in for a neighborhood bicycle theft. ”
Another hypothesis is that SARS CoV-2 binds to ACE-II receptors (or angiotensin converting enzyme II) in the blood and therefore is the entry point for the coronavirus. ACE-II is a protein found on the membranes of various cell types in the human body that includes alveoli in the lungs. Some studies show that the binding ability of the virus to these receptors in children is comparatively low, and thus the coronavirus is unable to attach to the alveoli in the lungs of the infants and children, preventing them from either getting infected or if infected, then with less severity than adults.
According to some researchers, children more frequently experience respiratory infections such as respiratory syncytial virus and, therefore, produce more antibodies against the virus as compared to adults. This abundance of antibodies in children could be protective when it comes to infections with coronavirus. On the other hand, over a period of many years, adults also experience many different types of respiratory infections and produce antibodies in their system. Then why don’t these antibodies protect them from coronavirus? Some researchers believe that due to the mutations in the virus over a period of time, the antibodies produced previously do not match with the newer strains of the virus. These unmatched antibodies in adults are unable to protect them from new viral strains.
While these hypotheses still need to be confirmed, they provide useful insights to the researchers in understanding the virology and in the development of therapeutics. There are dozens of companies and hundreds of scientists around the world who are working on developing the solution to combat the coronavirus in different and unique ways. I-Mab Biopharma is developing a neutralizing antibody, TJM2, to treat patients experiencing the Cytokine Storm. Gilead is working on Remdesivir – a nucleotide analog with broad spectrum antiviral activity. Moderna is approaching the problem with its mRNA (messenger ribonucleic acid) technology platform that alters the sequence of codes for the development of proteins inside the cells. Quantitative Biosciences Institute is mapping the proteins that virus thrives upon the human body and find ways to break that relationship. Some existing medicines, more notably the good old antimalarial drug – Chloroquine, are being tested for their efficacy in the treatment of coronavirus. Chloroquine and its derivative hydroxychloroquine can potentially prevent the viral attack by blocking the ability of the virus to enter the cell membrane or binding to the ACE-II receptors in the blood.
These are just a few examples of different ways in which scientists are fighting this battle with the COVID-19. Understanding the outbreak, transmission of virus and host responses to the infection present with valuable clues to researchers for the development of the solutions. The differences in host responses by age is another important aspect of the spectrum that can be helpful in this quest.
It should still be remembered that Jian and Mei may not have severe symptoms of coronavirus infection but they were still infected with the virus and had the ability to infect their elders and putting their lives at risk.
Sources
World Health Organization
The Lancet
The New England Journal of Medicine
The Journal of the American Medical Association